UPMC and Pitt will participate in a clinical trial to study the safety and effectiveness of a new brain-computer interface (BCI) to help people with severe paralysis. The National Institutes of Health (NIH) has awarded a $10M grant to initiate the COMMAND U.S. clinical trial of a motor neuroprosthesis to Carnegie Mellon University, UPMC, Mount Sinai Health System and Synchron collectively.
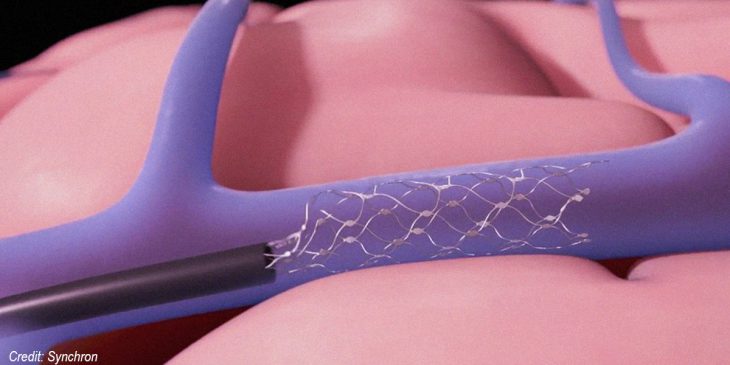
The Stentrode, developed by Synchron Inc., is implanted through a minimally invasive procedure using a catheter to place the device in a large vessel near the brain’s primary motor cortex. The device is wireless, mobile, fully implantable and does not depend on robotic limbs to reap the full benefit – unlike other BCIs currently in use.
For people living with paralysis, like those with amyotrophic lateral sclerosis (ALS) or stroke survivors, performing everyday tasks is a struggle. The Stentrode technology picks up brain signals, then transmits them to a small unit placed in the chest. The chest device is connected to an external receiver that converts the brain signals into commands and sends them wirelessly to a computer, allowing the patient to control it through thought.
“The hope is that this portable technology, that does not require opening the skull, can be used to generate speech in real-time and perform numerous other computer-generated tasks to enhance the quality of life in patients with ALS and other conditions in which use of the limbs and speaking are limited,” said Dr. David Lacomis, the co-principal investigator at UPMC/Pitt and a professor of neurology and pathology at Pitt.
UPMC and the University of Pittsburgh’s Rehab Neural Engineering Labs (RNEL) will work together to recruit patients. They will work with Carnegie Mellon University (CMU) – which is taking the lead in the management of the grant – and Mount Sinai Health System.
CMU will work with Synchron to explore machine learning methods for processing and decoding brain signals to detect the user’s intended actions and a haptic feedback interface for improving speed and accuracy of BCI control. UPMC and Mount Sinai Health System will collectively recruit eligible patients, perform the minimally-invasive neurointervention procedures and monitor the subjects’ clinical status.
This new trial will build on the results of an Australian study, published in the Journal of NeuroInterventional Surgery, which showed that two Australian patients implanted with the Stentrode learned to control texting and typing through direct thought. After training on mouse-clicking, they used the system unsupervised in their homes to send text messages, shop online and manage their finances.
Researchers expect to implant the device in the first U.S. patient within the next 12 months.