Even for the most attentive patients, it’s impossible to learn all the names of those involved in the course of their care.
Some are front and center — doctors, nurses, patient care support, environmental services — but others do crucial unseen work from behind the scenes — health information management, dietary and nutrition, maintenance and facilities.
And others, well, they’re even a bit further out of sight. Which actually might not be a bad thing, because for a few hundred patients a year, if they knew these names, it might draw a few quizzical looks.
After all, is there a reaction more appropriate than befuddlement to discovering that your shoulder repair, facial reconstruction surgery, or complicated tumor removal is thanks to something called Nifty Toad?
Or Unruffled Sloth, Constant Viper, Witty Chiton,* Immense Frog, or Wily Oryx ** for that matter?
Despite the fanciful animal monikers, these aren’t Pokémon or Disney characters. They’re some of the names given to the dozen 3D printers that make up the UPMC 3D Printing Program, which has been quietly but increasingly shaping patient-centered care across the system.
The printers’ quirky names come from the manufacturer, which bestows adjective-animal combos to every printer in lieu of a serial number. No matter what you call them, though, their impact can be measured in the hundreds of precise, patient-specific three-dimensional models used for everything from perioperative planning to teaching-training tools to patient education — as well as more recent expansions into surgical tools and guides, and on-demand substitutes for components to overcome crucial supply chain shortages.
These machines’ unassuming silhouettes — they look like Tesla decided one day to try its hand at making microwaves and air fryers — and the fact they’re whirring away in the back corridors of UPMC Presbyterian, mean few patients or staff are aware of the revolutionary potential of 3D printing.
“It’s really a game-changer,” says Dr. Anish Ghodadra, assistant professor, Interventional Radiology and Bioengineering, and founder and medical director, UPMC 3D Printing Program.
‘You Saw the Light Bulb Go Off’
Game-changing innovation can, and does, take many forms at UPMC.
In this particular case, innovation looks a lot like the shelves of a windowless room packed with scale models of skulls, aortas, tumors, hearts, and shoulder joints. To a casual observer, the models could be confused with generic training devices. In reality, they are far, far from that.
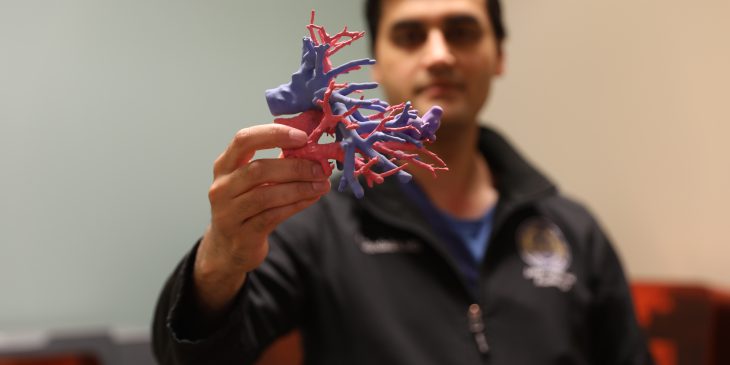
Ghodadra, a 39-year-old with an easy smile who began his career in medical device engineering before moving to Interventional Radiology, lifts one of the models off the shoulder-height shelf.
“When we talk about patient-centered care,” he says, lifting the model a little higher for emphasis, “this is the conduit to patient-centered care.”
He returns the model and points at others on the shelf, not entirely unlike a proud parent pointing out each member in a family photo.
“This is this patient’s kidney, this is that patient’s malformation, this patient’s liver veins — this is what they are,” he says. “We’re creating tools that are patient-specific, patient-centered, that improve outcomes, improve quality.”
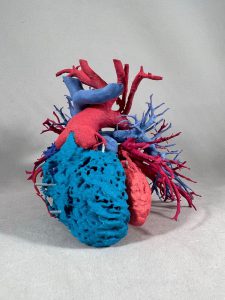
That’s because every clinical model produced by the 3D Printing Program is created from a patient’s actual two-dimensional CT scans, which become three-dimensional virtual models, which are then precisely printed physical models recreated in resin down to 0.2 mm.
CT scans have long allowed providers insight that, prior to their adoption, had never been possible. But when you look at CT scan on a computer and you scroll through images, Anish says, you are forced to “try to kind of mentally reconstruct in your head” what the images represent.
“It’s imagination at that point,” he says.
A 3D model — which is printed at no added cost to patients — has all the information of a CT scan but in a more accessible form. Going from a two-dimensional image to a model you can hold in your hand eliminates the cognitive effort needed for “translating from the screen to the physical world — even for folks who look at CT scans every day,” he says.
“You know the old saying that a picture is worth a thousand words?” Ghodadra says. “What is a physical model worth?”
Ghodadra lifts a palm-sized peach and purple model of a kidney with a sickly green-shaded tumor protruding from the top. He splits it in two — magnet clasps had held together each half — revealing the rest of the tumor, nestled amongst a tangle of red and blue arteries and veins inside the organ.
“These are physical representations, and we are physical creatures who live in a 3D world,” he says. “At a very fundamental level, it’s much easier for us to understand and grasp.
“If I hand you a physical object, you’re taking in visual data and your haptic and proprioceptive data,” he says. “Holding it, turning it over in your hand, you can get an instant, intuitive understanding of what’s going on.”
That particular benefit has been apparent ever since the first clinical model Ghodadra created — a splenic artery aneurysm — helped settle a debate among interventional radiologists as to how to proceed with treatment.
“I remember handing this to the treating physician, and he looked at it and he goes, ‘oh, I know what to do now,’” he says. “You saw the light bulb go off.”
‘An Instrumental Part of My Practice’
There are numerous clinical applications for the models — “I could go on and on,” Ghodadra says — but one of the original goals of the 3D Printing Program was improving providers’ periprocedural planning.
The models have done so by helping providers know where they can make incisions or where they can drill without complication, by allowing them to pre-bend plates for reconstructive surgery, or by giving them a chance to put the scope into the model and take a practice run at a procedure.
The ability to practice a procedure or plan specifically for a patient’s unique anatomy provides immense benefits, says Dr. Carl Snyderman, Otolaryngology director, Center for Cranial Base Surgery.
“3D-printed models are invaluable in visualizing [complex anatomical] relationships and developing a mental road map for surgery,” he says.
In addition to improving outcomes of individual cases, the models have also proven to be a boon for teaching and training Ghodadra says, by allowing residents and fellows to tangibly experience difficult or rare cases.
“These are the types of cases where you may only see one or two of these in real life in five years,” he says, “but I can let you literally practice on ten of them.”
Dr. Noel Jabbour, residency program director, Otolaryngology—Head and Neck Surgery, says the printed models have positively impacted training at UPMC Children’s.
“The 3D Printing Program has allowed us to execute a deliberate practice curriculum where our residents spend many hours learning the skills of surgery outside of the operating room, making them game-ready before they start to practice on real patients,” he says.
In addition to benefiting teaching and training, when a model is prepared ahead of surgery, providers can sit down with the patient to describe — and show — how the team is going to approach the procedure, which enhances the patient experience, Ghodadra says.
“Imagine going to a patient nervous about surgery and say, ‘actually I did it yesterday,’” he says. “It’s really profound [for patients] to touch, and feel, and get a sense of what’s going on.”
That’s been the experience of Dr. Amanda Stapleton, pediatric otolaryngologist and endoscopic sinus and skull base surgeon, UPMC Childrens, who says the models have become “an instrumental part of my practice” because she can use them to describe to a pediatric patient’s family just what an upcoming procedure will entail.
“I show them how we are going to take the lesion out and what structures we need to protect,” she says. “The families love the models — it really helps them understand what their child is going through — and it gives them more confidence in the surgical team.”
‘It Makes Surgery Better’
The 3D Printing Program’s clinical models are frequently requested for the treatment of trauma, cancer, aneurysms, and cardiac issues.
Models can be printed with key information color-coded or with flexible materials, which allows them to be used for a multitude of procedures, like to plan implantation of electrodes to treat seizures or to determine the configuration of a particular patient’s atrium or to practice drilling into the air cells within a child’s temporal bone to place a cochlear implant without harming the facial nerve.

And for complex surgical procedures, the models can improve outcomes by giving surgeons information that otherwise wouldn’t have been available until after a procedure began, says Dr. Adam B. Christopher, director of cardiac MRI and CT, UPMC Children’s Hospital.
“3D representation of congenital heart disease has allowed us to convey complex spatial relationships that were previously understood only at the time of a procedure,” he says.
Having that information before going into the OR has improved accuracy and efficiency, he says.
Ghodadra says about half their models are created for orthopedic procedures that involve altering anatomical structure, like shoulder or hip surgeries and trauma reconstructions.
“We have shoulder surgeons who will not operate without one of our models,” Ghodadra says. “It’s almost become standard of care.”
Ghodadra says that’s because these types of “very physical, very tactile” surgeries can be performed first on a printed model to determine the best course and then can be recreated on the actual patient using 3D-printed surgical guides and pre-formed plates, thanks to a dedicated suite of printers operated in a clean setting that can produce biocompatible materials for use directly in the operating room. Research shows using models like this saves an average of 45 minutes.
“That’s 45 minutes less anesthesia for the patient because they’re open less,” he says. “It makes surgery better.”
‘There’s Just So Much You Can Do’
Started in 2016 when it was a single printer and “just me tinkering in a closet,” Ghodadra says, the 3D Printing Program has grown to include three full-time engineers and a yearly output of around 400 clinical models.
Initially funded by a Frontline Innovation Grant from the Beckwith Institute, the program has expanded beyond its original goal of creating patient-specific models for preoperative planning and trainee/patient education.
“It’s actually one of the problems that we have,” Ghodadra says, “there’s just so much you can do.”
Sitting in his office at Presby, Ghodadra is surrounded by reminders of how far the 3D Printing Program has grown.
A plethora of models occupy nearly every horizontal surface — including a printed version of his own child’s ultrasound. Though the entire 3D Printing Program is set to relocate to a centralized space in another building in late fall, it’s easy to imagine any future space would also soon be dotted with resin replicas.
That new space will likely also feature a different kind of keepsake, which for now sits on the floor, nestled next to a file cabinet, underneath a white board, and just in line with the visitor’s chair. Its clear plastic front is adorned with a nametag on its bottom lefthand corner: Big Finch.
“It was the first printer I ever bought,” he says, with a grin and a slight lift of his shoulders. “I couldn’t bear to part with her.”
*A Chiton is a marine mollusk that looks kind of like a pill bug. Yes, we had to look that up.
** Yes, this also required a Google search. You’ll probably recognize them as the straight-horned antelopes from the Lion King.
Journalists interested in learning more can contact mediarelations@upmc.edu.