Could vision, once lost, ever be regained? From using gene therapies to implanting pinhead-size electronic chips in the retina, Pitt scientists are making great progress at creating a hopeful future for those affected by vision loss.
Dr. Xing Chen is a neuroscientist who joined Pitt’s Department of Ophthalmology as an assistant professor late last year. Her ultimate research goal is ambitious: Chen wants to restore lost sight by directly stimulating the brain and hopes to turn visual prostheses from a sci-fi concept into reality within the next six years.
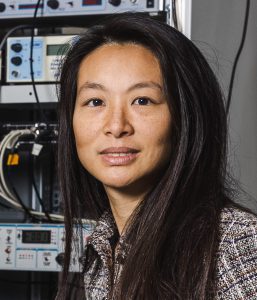
Dr. Xing Chen
In her latest study, which was published in the Journal of Neural Engineering earlier this month, Chen developed and tested a neuroprosthesis system with many times more electrodes than anything attempted by other research groups ever before, allowing monkeys to recognize artificially generated letters. Chen is gradually refining and improving the existing technology by pushing the system to its limit, with the intention of restoring rudimentary vision in blind people.
The idea that direct brain stimulation could one day produce full-fledged artificial vision has existed for nearly a century. But practical applications of this technology are yet to materialize, though other related fields are much closer to succeeding.
Brain-computer interfaces, or BCIs, for example, are becoming widely used in innovative research on restoring lost function after partial or full paralysis due to severe brain or nerve tissue damage, whether from stroke or a car accident.
Other studies from Pitt showed that a BCI consisting of four electrode arrays implanted in the motor and sensory regions of the brain cortex can help a paralyzed man control a robotic arm. Other groups in Europe showed that a BCI can help a man walk again. Still, development of visual BCIs that may one day supplement or even replace natural vision remains nascent, despite being studied since the 1960s.
The main problem, Chen says, is that vision is incredibly complex: “The bandwidth of information that comes in via our eyes is extremely high – our eyes detect signals from millions of ‘pixels,’ and a large area of our brain is involved in the generation of vision. Replicating that with a BCI is very difficult.”
A slew of exciting research trials, including a study of using light-sensitive algae proteins to restore lost function of the retina, are already bringing hope to people blinded by previously uncurable genetic disorders. But there is still no solution for people who lost sight due to extensive damage to their eyes or the optic nerve.
Chen’s research is poised to change that.
By stimulating specific electrodes across arrays implanted in the visual cortex, researchers can trick the brain into “seeing” dots of light appearing across the visual field. When put together, those dots, called phosphenes, eventually combine into mental images resembling crude shapes and, with enough resolution, render more detailed images.
Clinical experiments published in the last two years showed some success in evoking visual perceptions of simple shapes, such as circles and lines, by stimulating the visual cortex in the back of the brain of a blind human volunteer. But obtaining the kinds of vivid and detailed images that are brought to us by natural vision would require stimulating dozens of electrodes at once.
As the first step in developing a high-resolution visual neuroprosthetic, Chen wanted to see if she could safely increase the number of implanted electrodes from 96 to 1,024 and whether the device could be left implanted for much longer than what was attempted previously – up to three-and-a-half years instead of six months.
Spanning the area of eight square centimeters across the visual cortex in the back of monkeys’ brains, the system consisted of 16 tiny microelectrode arrays that could both record from and stimulate brain areas chosen by the investigators. After years of meticulously monitoring the signal quality and tweaking stimulation parameters to achieve reliable evocation of phosphenes exactly where the researchers wanted them to appear, Chen and her team identified several possible challenges that lie ahead.
For instance, while the monkeys remained healthy throughout the study and the device itself remained intact and capable of delivering stimulation, the signal quality gradually degenerated after two years.
“Due to differences in brain and skull anatomy between humans and monkeys, our results don’t rule out the possibility that large numbers of arrays might be useful for vision restoration in humans,” Chen noted. “We are already making modifications to implant design and look forward to using our new knowledge to improve the system and make it as safe and powerful as possible.”