Three Lakes Foundation has selected the University of Pittsburgh and Yale schools of medicine to lead a consortium to accelerate research into understanding and treatments of pulmonary fibrosis (PF). Pitt’s School of Medicine will receive a grant to develop and refine a new model to better understand the progression of PF and to identify possible therapies.
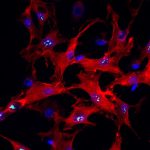
Structure of a healthy lung.
Credit: University of Pittsburgh
PF is a chronic, degenerative lung disease that causes lung tissue to become damaged and scarred, making it difficult for oxygen to enter the bloodstream. Each year, 40,000 Americans die from PF, yet very little is known about the mechanisms of the disease.
“I wanted to understand how diseased lungs can look so different from healthy lungs,” said Dr. Melanie Königshoff, visiting professor of medicine at Pitt and lead investigator of the consortium.’’ To create the models, she and her team leveraged UPMC’s robust lung transplant program and the Simmons Center for Interstitial Lung Disease to receive lungs being removed from patients, as well as small pieces of donor lungs. Then the team takes a slice of tissue small enough to be viewed under a microscope but large enough to maintain the three-dimensional architecture of the organ.
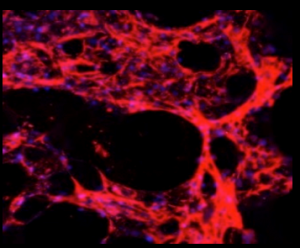
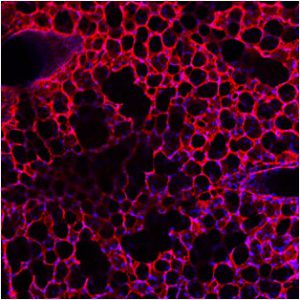
Structure of lung with pulmonary fibrosis. Credit: Universtiy of Pittsburgh
With these slices, Königshoff can make healthy tissue sick with PF, allowing her team to watch up close as the disease advances.
However, human lungs are a limited resource, and many research institutions don’t have access to a transplant center. Dr. Kambez H. Benam, visiting associate professor at the University of Pittsburgh School of Medicine and co-investigator on the consortium, hopes to take the information the team learns from the human models and use it to create 3D-bioprinted models.
“Using emerging technologies like 3D printing to create these models allows researchers around the world to more easily study the progression of these lung diseases,” Benam said. “It also allows more scientists to test potential treatments.”
There are currently no effective treatments for PF, but these models may give researchers the insights they need to develop or identify one.
The COVID-19 pandemic has only increased the need for a deeper understanding of and more effective therapies for chronic lung conditions. As more people recover from COVID-19, therapies for living with the long-term effects of the disease become increasingly important.
“We know that once patients recover from COVID-19 disease, pulmonary fibrosis can develop,” said Königshoff. “We hope to be able to use these models to better treat these chronic lung conditions, but also one day study the effects of the virus itself.”