When Dr. Sarah Gaffen first opened her laboratory in 1999, the number of peer-reviewed research papers about IL-17 – a family of pro-inflammatory substances secreted by our immune cells – could be counted on one hand.

Drs. Sarah Gaffen and Partha Biswas at a Black Lives Matter demonstration.
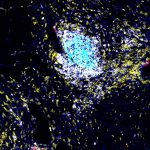
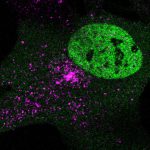
Now academic publications involving IL-17 number in the tens of thousands, and Gaffen and her colleagues recently added two key articles to the list, cracking the code for how IL-17 activates a cascade of cellular signals leading to inflammation in kidney disease. Their finding could ultimately lead to targeted medications for the growing number of people with the disease, which now afflicts 15% of U.S. adults.
“For me, this discovery is so exciting because it’s the culmination of more than two decades of work for my lab,” said Gaffen, the Gerald P. Rodnan Endowed Professor in the Division of Rheumatology and Clinical Immunology at the University of Pittsburgh School of Medicine. “This discovery goes all the way back to the very first paper we ever published on IL-17, where we saw that one of the most potent IL-17-dependent genes was involved in kidney function, but we didn’t understand how the system worked. Now we do.”
Gaffen – whose web site outlines her lab philosophy of scientific integrity, diversity, inclusion, respect and a belief “that the number 17 is awesome” – joined forces with Dr. Partha Biswas, associate professor of rheumatology and clinical immunology at Pitt, and his lab, which centers its research on IL-17 signaling in the kidney.
“Kidney disease is often overlooked, but it’s the ninth-leading killer disease in the world – and it’s on the rise because it can be caused by diabetes and high blood pressure,” said Biswas. “Understanding kidney disease, in particular chronic and inflammatory kidney disease, is very important to developing therapeutic strategies.”
Together, Biswas and Gaffen found and described the meticulous genetic instructions that encode a transcription factor – or “power switch” – that turns on and off the production of IL-17 in the kidney. The good news is that existing medications used for other diseases may be able to flip that switch.
That does not mean those medicines can immediately be used for kidney disease in humans. Gaffen and Biswas, who are basic scientists, are sharing their laboratory findings with the long-term goal that clinical scientists can translate this research into patients in a clinical setting.
“Without a deep understanding of the fundamental molecular mechanisms operative in inflammation, we’re working in the dark,” said Gaffen.
Learn more about the teams’ research in their recently published papers in Science Immunology and JCI Insight.