UPMC’s Critical Illness Recovery Center is helping survivors of ICU stays manage PostIntensive Care Syndrome, a complex set of physical, emotional and cognitive symptoms. In a new JAMA documentary, ICU survivor Ken Foltz shares how Dr. Brad Butcher and the UPMC team guided his recovery.
For Ken Foltz, leaving the intensive care unit (ICU) after battling sepsis wasn’t a return to normal. It was the beginning of his new life as a survivor.

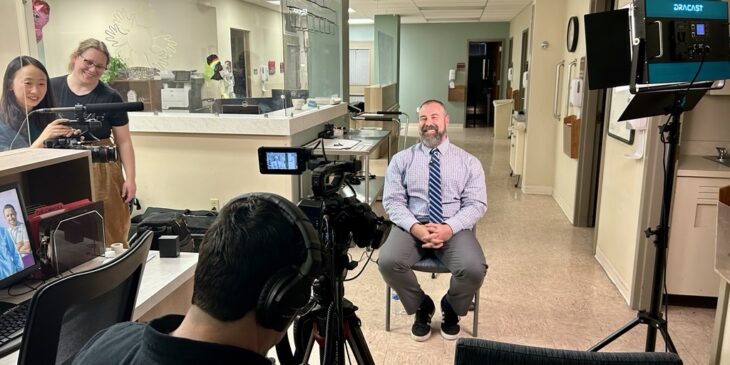
Ken Foltz, center in white hat, and other Post-Intensive Care Syndrome (PICS) patients and advocates at the Walk4PICS awareness event.
Ken is one of more than half of ICU patients who experience symptoms of post-intensive care syndrome (PICS), which emerge during and after an ICU stay. They can affect every part of a person’s life and include cognitive, physical, emotional and social manifestations.
A former attorney-turned-advocate, Foltz shares his experience with PICS and his goal-oriented recovery – aided by the UPMC Mercy Hospital’s Critical Illness Recovery Center (CIRC) – in a new documentary produced by JAMA News.
“I’m not going to go back to being the person I was, that’s just not reality,” said Foltz, explaining that by working with the team at UPMC Mercy’s CIRC he learned what to expect after leaving the ICU and that just because he wasn’t snapping back into his old life, he wasn’t “failing” at recovery.
“One of the things, working with the folks at CIRC early on, that was so incredibly helpful for me, was literally them explaining to me what PICS was,” he said.
Dr. Brad Butcher gives a speech outside of UPMC Mercy Hospital during the Walk4PICS awareness event.
What is Post-Intensive Care Syndrome (PICS)?
Dr. Brad Butcher, associate professor of critical care medicine at the University of Pittsburgh School of Medicine and intensivist at UPMC, explained that, although PICS occurs in at least 54% of patients who had an ICU stay, there isn’t one definitive cause or a specific treatment. Rather, treatment is focused on learning the patient’s recovery and life goals and then mapping a clinical plan to help them achieve those goals.
How UPMC Mercy’s Critical Illness Recovery Center Supports ICU Survivors
The UPMC Mercy CIRC is one of the first of a small number of similar clinics worldwide that gather an array of specialists who – over the course of several hours – see patients after their ICU stay and then collaborate on a care plan moving forward. The clinical team can include a critical care doctor or advanced practice provider, nurse, pharmacist, respiratory therapist, speech and language pathologists, physical and occupational therapists, social worker and a dietician.
“This is probably the longest doctor’s appointment that you will have ever had and will likely ever have in your life. You’re going to see a lot of people,” Butcher said.
Treating PICS is an emerging field and research publications are rising exponentially, said Butcher, who has been studying and presenting about the syndrome and the UPMC Mercy CIRC model for nearly eight years. Many ICU survivors report feeling that clinics like the CIRC greatly benefit their recovery, and clinician-scientists in this new field are working diligently to determine which patients these clinics can help the most and what type of care is most appropriate.
“It really is an emotional experience when you’ve rescued someone from an otherwise certain death and paired up with them in the outpatient setting to become their teammate in their recovery journey,” Butcher said. “It’s what medicine is meant to be.”
Learn more about PICS, ICU recovery and UPMC Mercy’s Critical Illness Recovery Center: