A year ago, when U.S. health authorities issued their first warning that COVID-19 would cause severe “disruption to everyday life,” doctors had no effective treatments to offer beyond supportive care.
There is still no cure, but thanks to an unprecedented global research effort, several treatments are helping patients survive COVID-19 and stay out of the hospital altogether.
COVID-19 treatments target two broad problems: the coronavirus’s ability to spread through the body, and the damage caused by the body’s immune system response. When the virus enters the body, it takes over cells and uses them to replicate itself. In response, the body sends inflammatory signals and immune cells to fight the virus. In some patients, that inflammatory response can continue even after the virus is under control, leading to damage in the lungs and other organs.
The best tool is prevention, including using face masks and vaccines. Vaccines train the immune system to fight off attackers. With less risk of an uncontrolled infection, they can cut the risk of death from COVID-19 to near zero. But vaccine supplies are limited, even with a third vaccine now authorized for U.S. use, so treatments for infected patients remain crucial.
As doctors who work with COVID-19 patients, we have been following the drug trials and success stories. Here are six treatments commonly used today for COVID-19. As you’ll see, timing matters.
Treatments that can keep you out of the hospital
Two promising types of treatments involve injecting antiviral antibodies into high-risk COVID-19 patients before the person becomes severely ill.
Our bodies naturally create antibodies to recognize foreign invaders and help fight them off. But natural antibody production takes several days, and SARS-CoV-2 – the coronavirus that causes COVID-19 – replicates fast. Studies show that injecting patients with antibodies soon after symptoms begin can help protect patients against serious infection.
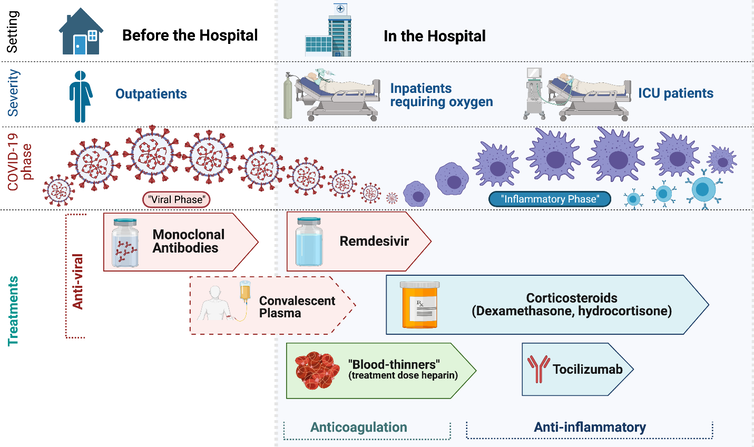
Treatments for COVID-19 and their timing.
Georgios D. Kitsios, CC BY-ND
Monoclonal antibodies: These lab-engineered antibodies can bind to SARS-CoV-2 and prevent the virus from entering cells and infecting them. They include Bamlanivimab and the combined therapy casirivimab/imdevimab developed by Regeneron. The U.S. Food and Drug Administration granted emergency use authorization for these therapies because they have been found to protect high-risk patients from hospitalization and death. Once patients are sick enough to need hospitalization, however, studies haven’t found a proven benefit from them.
Convalescent plasma: Another way to deliver antibodies involves blood drawn from patients who have recovered from COVID-19. Convalescent plasma is primarily given in research settings because the clinical evidence so far is mixed. Some trials show benefits early in the disease. Other studies have not shown any benefit in hospitalized patients.
There may be a role for convalescent plasma as a supplemental therapy for some patients because of the growing threat of mutated SARS-CoV-2 variants, which may evade monoclonal antibody therapy. However, careful research is necessary.
Treatments for hospitalized patients
Once patients become so sick that they have to be hospitalized, treatments change.
Most hospitalized patients have difficulty breathing and low oxygen levels. Low oxygen occurs when the virus and corresponding immune response injure the lungs, resulting in swelling in lung air sacs that restricts the amount of oxygen getting into the blood. Patients hospitalized with COVID-19 usually need supplemental medical oxygen to help them breathe. Doctors frequently treat patients on oxygen with the antiviral agent remdesivir and anti-inflammatory corticosteroids.

Most hospitalized COVID-19 patients have trouble breathing and getting enough oxygen.
AP Images/David Goldman
Remdesivir: Remdesivir, originally designed to treat hepatitis C, stops the coronavirus from replicating itself by interfering with its genetic building blocks. It has been shown to shorten the length of hospital stays, and doctors may prescribe it to patients on oxygen shortly after arrival in the hospital.
Corticosteroids: Steroids calm the body’s immune response and have been used for decades to treat inflammatory disorders. They are also widely available, cheap and well-studied medications, so they were among the first therapies to enter clinical trials for COVID-19. Several studies have shown that low-dose steroids reduce deaths in hospitalized patients who are on oxygen, including the sickest patients in the intensive care unit, or ICU. Following the findings of the landmark RECOVERY and REMAP-CAP COVID-19 studies, steroids are now the standard of care for patients hospitalized with COVID-19 who are treated with oxygen.
Blood thinners: Inflammation during COVID-19 and other viral infections can also increase the risk of blood clots, which can cause heart attacks, strokes and dangerous clots in the lungs. Many patients with COVID-19 are given the blood thinners heparin or enoxaparin to prevent clots before they occur. Early data from a large trial of COVID-19 patients suggests that hospitalized patients benefit from higher doses of blood thinners.
Some patients with COVID-19 become so sick that they need an ICU for high levels of oxygen support or a ventilator to help them breathe. There are several therapies available for ICU patients, but ICU patients have not been found to benefit from high doses of blood thinners.
Treating the sickest patients
ICU patients with COVID-19 are more likely to survive if they receive steroids, studies have found. However, low-dose steroids alone may not be enough to curb excessive inflammation.
Tocilizumab: Tocilizumab is a lab-generated antibody that blocks the interleukin-6 pathway, which can cause inflammation during COVID-19 and other diseases. New results from the REMAP-CAP trial that have not yet been peer-reviewed suggest that a single dose of tocilizumab given within one to two days after being placed on respiratory support reduced the risk of death in patients already receiving low-dose steroids. Tocilizumab has also been shown to benefit patients with high levels of inflammation in early results from another trial.
These innovative therapies can help, but careful supportive care in the ICU is also crucial. Decades of extensive research have defined core management principles for helping patients with severe lung infections who need ventilators. These include avoiding underinflation and overinflation of the lung by the ventilator, treating pain and anxiety with low levels of sedative medications, and periodically placing certain patients with low oxygen levels on their belly, among many other interventions. The same key principles likely apply to patients with COVID-19 to help them survive and recover from a critical illness that can last weeks or months.
Medical progress since the start of the pandemic has been awe-inspiring. Doctors now have vaccines, antiviral antibodies for high-risk outpatients and several treatments for hospitalized patients. Continued research will be crucial to improve our ability to fight a disease that has already claimed more than 2.5 million lives worldwide.![]()
This article is republished from The Conversation under a Creative Commons license. Read the original article.