Over 50 million people suffer from epilepsy worldwide, and while there is no cure, there are many drugs available to help manage disease. Yet scientists have not, until now, known how some anti-convulsant medications directly interact with their target proteins in the brain.
New research has mapped the exact location of these interactions for a widely used class of anti-convulsants, opening opportunities to develop even better anti-convulsant medications with higher efficacy and fewer side effects. The study, led by University of Pittsburgh post-doctoral associate Dr. Anshumali Mittal and Matthew Martin, a graduate student in the Pitt-Carnegie Mellon University molecular biophysics and structural biology program, was recently published in Nature Structural & Molecular Biology.
“Solving the structure of proteins provides atomic-level detail, which is very useful for trying to understand how they work,” said Dr. Jonathan Coleman, assistant professor in the Department of Structural Biology in the School of Medicine at Pitt, and senior author on the study.
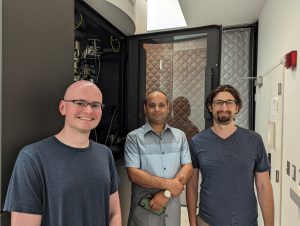
Researchers Matt Martin, Anshu Mittal, and Jonathan Coleman (left to right) in front of the Titan Krios electron microscope at the University of Pittsburgh
The lab resolved the structure of two key proteins implicated in epilepsy and synaptic transmission: SV2A and SV2B. Located in vesicles at the ends of neurons, at the synapse where neurons communicate, SV2A and SV2B are critical for brain function. They belong in a small family of synaptic vesicle proteins which includes a third member, SV2C.
Disruption of SV2A results in seizures, and while those proteins have been studied for years, their functions are not well understood. This is due to how difficult they have been to study with structural and biochemical techniques in the lab.
Coleman and his group focused on how to produce stabilized SV2A and SV2B and used innovative data collection methods to generate their structures.
“These proteins are very wiggly,” said Coleman. “They usually show up as a blur in our maps, so we used several tricks and tools to generate high resolution images.”
Working with scientists at UCB Pharma, a biopharmaceutical company headquartered in Belgium, the Coleman lab used nanobodies to stabilize SV2A and SV2B and generated cryogenic electron microscopy images of the proteins bound to anti-convulsant molecules. They found that anti-convulsant molecules bind to a conserved site in SV2A and SV2B, meaning the site is critical for protein structure and function, and therefore is highly similar amongst related proteins.
Another key goal of this project was to understand why some anti-convulsants preferentially bind SV2A, compared to SV2B and SV2C. By resolving the structure of both SV2A and SV2B, Coleman and his team found that specific residues which are only found in SV2A, mediate this binding. Coleman’s lab plans to use these structures to dive into protein function, notably, how these proteins work in the brain as transport proteins. This knowledge is particularly valuable for drug development and exploration of future targeted therapies.
“Until now there was no proof that this region was where drugs were binding,” adds Coleman. “This opens the door to develop drugs that target SV2A and SV2B.”
Kaleigh Connors is a Ph.D. candidate in the University of Pittsburgh School of Public Health Department of Infectious Diseases and Microbiology. She is participating in the UPMC Science Writing Mentorship Program.