A newly identified genetic marker could potentially predict which patients are likely to respond to immunotherapy in cancer types that have lacked such tools until now, according to a study published in Cancer Immunology Research, a journal of the American Association for Cancer Research.
Led by researchers at the University of Pittsburgh, the study found that tumors with greater number of difficult-to-detect rearrangements of their genetic code — known as intragenic rearrangement (IGR) burden — may respond better to immunotherapy. The findings could pave the way for more precise treatment decisions for patients with cancers such as breast, ovarian, esophageal and uterine.
“Immunotherapy has been a major breakthrough for cancer treatment, but only a small subset of patients respond favorably. The question is, how can we identify these patients?” said senior author Dr. Xiaosong (Johnathan) Wang, associate professor of pathology at Pitt and UPMC Hillman Cancer Center. “Genetic tests are available that are great at predicting immunotherapy response in melanoma and lung cancer, but they don’t work well in some other cancers. To help fill this gap, we developed a new approach, which analyzes a class of hidden, or cryptic, rearrangements in the cancer genome.”
Dr. Xiaosong (Johnathan) Wang
Correctly identifying which patients will respond to immunotherapy and those who will not is crucial because these immune-boosting treatments can cause severe immune-related side effects and may even accelerate cancer progression in some patients.
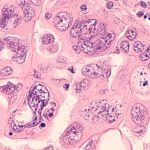
One approach to identify immunotherapy responders looks at the number of simple mutations in the DNA of cancer cells, known as tumor mutational burden (TMB). Because cancerous cells are derived from healthy cells in the body, they often fly under the immune system’s radar. When cancers have many simple mutations, or high TMB, they are more conspicuous, so T cells can better recognize and destroy these malignant cells. It’s these tumors with high TMB that make a patient a good candidate for immunotherapy, but this test only works well for highly mutated cancers such as melanoma and lung cancer.
In search of a new genetic biomarker that would predict immunotherapy success for other cancers, Wang and his team used a large database from the International Cancer Genomic Consortium to analyze more than 1,000 cancer genomes, spanning a wide variety of cancer types. They showed for the first time that measuring the overall burden of IGR could potentially predict immune cell infiltration and immunotherapy response in certain types of cancer.
IGR results from cryptic structural rearrangements of a cell’s genetic code, or genome, within a gene. In this analogy, if the genome is represented by an encyclopedia and a gene is an entry, IGR burden is the amount of duplications, deletions or relocations of entire paragraphs within entries. In contrast, TMB is like the number of simple typos, or words that have been misspelled by one or few letters.
“TMB, which measures simple mutations has been intensively studied, whereas IGR represents the dark side of cancer genetics because these aberrations are cryptic and difficult to study,” explained Wang.
Wang and his team first looked at the relationship between IGR and TMB in different tumor types. They found that cancers with high TMB, such as melanoma and lung cancer, had low IGR burden. Vice versa, breast, ovarian, endometrial and esophageal cancers had relatively low TMB but high IGR burden.
Either high IGR burden or high TMB correlated with elevated measures of T cell inflammation, indicating that elevated levels of either type of genetic abnormality allow immune cells to recognize and possibly destroy cancers more easily.
“Our findings point to the existence of two distinct classes of cancers: those driven by simple mutations, or TMB-dominant, and those driven by intragenic rearrangements, or IGR-dominant,” said Wang. “This suggested to us that patients who don’t qualify for immunotherapy because of low TMB might still benefit from the treatments if they have high IGR burden.”
To test the hypothesis that high IGR burden is associated with immunotherapy response in IGR-dominant cancer, the team examined a clinical trial dataset of patients with esophageal cancer who were treated with the immunotherapy drug durvalumab. Indeed, patients with higher IGR burden responded better, and those with disease relapse tended to have lower IGR burden.
Wang and his team also analyzed a clinical trial dataset of bladder cancer patients being treated with the immunotherapy drug atezolizumab. As bladder cancer is a TMB-dominant cancer type, they found that TMB, but not IGR burden, predicted response and survival following atezolizumab treatment, as expected. However, among patients whose tumors were exposed to platinum-based chemotherapy before atezolizumab, IGR burden of the samples collected after platinum, but not before platinum, predicted immunotherapy response, possibly because platinum exposure may damage DNA and induce these structural rearrangements of the genome.
According to Wang, the findings highlight how IGR test results could be used by clinicians in different cancer types and contexts to help decide on the best treatment for a patient in the future. As the cost of whole genome sequencing has dramatically reduced — with $100 genome sequencing expected soon — measuring IGR burden could be feasible and affordable in the near future.
The researchers are now working to further develop and standardize their test and algorithm for clinical use.
Journalists interested in learning more can contact mediarelations@upmc.edu.