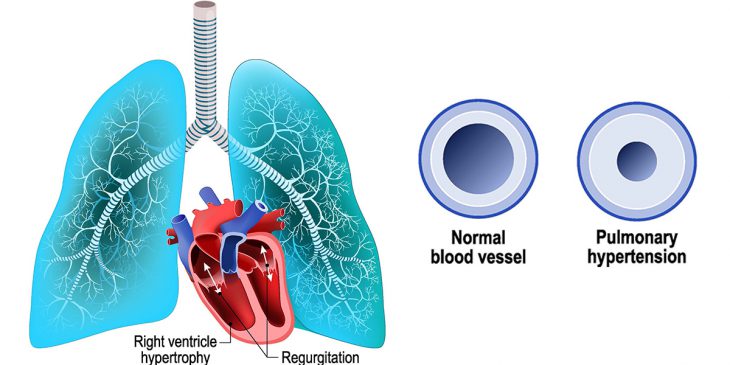
Pulmonary hypertension, or high blood pressure in the arteries of the lungs and heart, affects more than 10 million Americans and millions more worldwide. While there are some medications for specific types of pulmonary hypertension, there is no treatment that prevents or reverses the disease. There is no cure because currently, little is known about the true origins of the disease.
Pulmonary hypertension, which makes it difficult for your heart to pump blood due to narrowed and hardened arteries, results in shortness of breath and exercise intolerance, but over time, it can progress to heart failure and death. More effective detection and treatment strategies could be developed if progress can be made in understanding the disease at the molecular level.
New UPMC research from the laboratory of Dr. Stephen Chan, published today in the journal Circulation, demonstrates that mutations in a gene called BOLA3 can lead to a syndrome that results in pulmonary hypertension in affected individuals. Prior to this study, it was entirely unclear how BOLA3 deficiency could drive PH. BOLA3 has been linked to the metabolism of the amino acid glycine, which is known to be elevated in patients with pulmonary hypertension, but with unclear significance to the disease.
Over the course of three years, using a combination of state-of-the-art experimental strategies including the study of rare cells from patients with the BOLA3 mutation and special human and animal disease models of pulmonary hypertension, the Chan lab defined BOLA3 as a crucial regulator of glycine production from blood vessels in the lung, with a direct impact on PH development.
“These results provide a molecular explanation for the puzzling clinical and genetic associations linking pulmonary hypertension with high glycine,” said Chan, director of the Center for Pulmonary Vascular Biology and Medicine at the University of Pittsburgh and UPMC. “Based on these results, future work can utilize glycine as a testable marker to diagnose pulmonary hypertension, potentially early on in the disease process.”
Furthermore, altering glycine metabolism or decreasing glycine levels could be explored as a therapeutic option for pulmonary hypertension.
“This work supports the growing likelihood that genetic testing of mutations that predispose to pulmonary hypertension could be instrumental in identifying a currently undefined population of individuals at-risk for developing this devastating condition,” said Chan.
Visit the UPMC website for additional information on pulmonary hypertension.
To get more stories like this directly to your inbox, subscribe to our weekly Inside Life Changing Medicine newsletter at bit.ly/upmc_newsletter.