A protein responsible for lethal liver disease in mice infected with Rift Valley fever virus (RVFV) has been identified by scientists at the University of Pittsburgh Center for Vaccine Research. These results from new research published in Science Advances lay the groundwork for future vaccine development, as scientists are now one step closer to uncovering how RVFV multiplies within the body.
RVFV is a mosquito-transmitted virus found in Africa and known for its ability to infect wide ranges of animals, insects and humans. Although deadly in most animals, RVFV usually causes milder symptoms in humans but can lead to such complications as loss of vision, liver disease and encephalitis. Scientists have yet to create a vaccine or approve any drugs for treatment.
“The way in which viruses like RVFV can infect wide ranges of species is not well-understood,” said Dr. Amy Hartman, associate professor of infectious diseases and microbiology at Pitt’s School of Public Health. “If RVFV were to emerge in the U.S., it would be highly concerning due to how fast it can spread. Our ultimate goal is to use this research to create a vaccine for protection.”
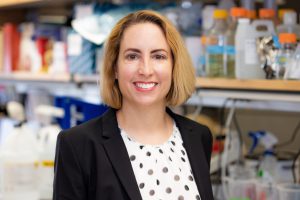
Dr. Amy Hartman
The liver is a major site of viral replication for viruses like RVFV. In her previous research, Hartman and her colleagues found that a cholesterol receptor found throughout the body, called low-density lipoprotein receptor-related protein 1 (Lrp1), was responsible for initiating the RVFV infection in animal cells. However, the role of Lrp1 in hepatic disease, as well as how the virus spreads and infects specific groups of cells within a living organism, remained major unanswered questions until now.
To study the interaction, Hartman and her colleagues at Washington University in St. Louis created mice that lack the Lrp1 receptor. Although Lrp1 could not be removed from the entire body — as doing so would cause immediate death — Hartman and her colleagues removed Lrp1 solely from the liver to see if the mice would still develop lethal hepatic disease if infected with RVFV.
For the liver-specific knockout mice, there was little to no viral replication of RVFV in the liver. These mice also lived twice as long as mice with intact Lrp1 levels in the liver. Although the Lrp1-knockout mice did not contract lethal RVFV hepatic disease, they eventually went on to develop a neurological disease mediated through the Lrp1 in their brains.
“Our results are important because they showed that Lrp1 is responsible for lethal RVFV liver disease in a mouse model,” said Hartman, who is also a member of the Center for Vaccine Research. “We can translate these results — as the liver is also responsible for viral replication in humans — and we now have the capability in future research to dissect how the virus spreads throughout the body.”