We interview Dr. Alan Wells, medical director of the UPMC Clinical Laboratories, to get answers to some frequently asked questions about antibodies, the tests used to detect them and why these tests are important during the COVID-19 pandemic.
What are the different types of COVID-19 tests?
There are two basic types of laboratory tests for COVID-19 – viral RNA tests and antibody tests.
 The U.S. Centers for Disease Control and Prevention, UPMC and many public and private labs around the world have created viral RNA tests for COVID-19. These tests use a tried-and-true molecular biology method to detect RNA – the single-stranded cousin of DNA – from the virus that causes COVID-19. These tests are run on mucus samples, ideally swabbed from deep inside the nose, or if a person has developed pneumonia, the sample can come from the fluid in the lungs.
The U.S. Centers for Disease Control and Prevention, UPMC and many public and private labs around the world have created viral RNA tests for COVID-19. These tests use a tried-and-true molecular biology method to detect RNA – the single-stranded cousin of DNA – from the virus that causes COVID-19. These tests are run on mucus samples, ideally swabbed from deep inside the nose, or if a person has developed pneumonia, the sample can come from the fluid in the lungs.
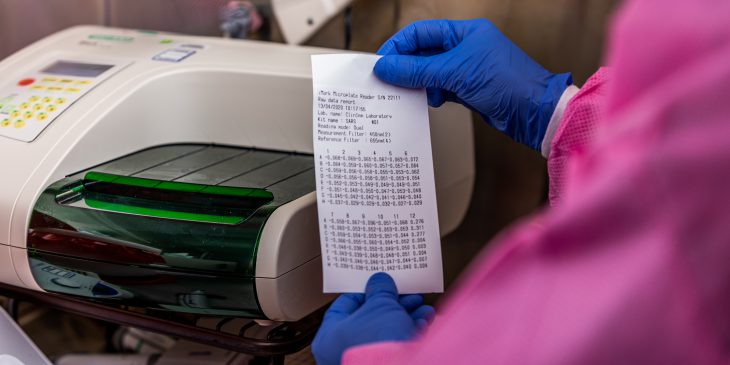
Antibody tests, which are currently being developed by many private companies, detect the body’s immune response to the virus by measuring COVID-specific antibodies in the blood.
Why does it matter whether you’re measuring viral RNA or antibodies?
Viral RNA tests return a positive result only as long as the virus is present in a person’s respiratory tract. Once the person recovers, this type of test can no longer determine whether they had COVID-19 versus some other respiratory illness.
On the other end of the spectrum, antibodies arise many days, even weeks, after the viral infection starts, and then they may persist indefinitely. An antibody test is not able to tell whether a newly infected person is harboring the virus, but it could be useful for identifying whether someone was previously infected, perhaps with mild enough symptoms that they didn’t even know they were sick.
At this time, we don’t know whether the antibodies being detected by these tests are neutralizing antibodies – meaning the type that can stop the virus from continuing to spread throughout the body – so it’s unclear whether a positive antibody test would indicate that the person is immune to the virus. At this point, there’s no definitive test for COVID-19 immunity.
How do these different tests contribute to controlling the spread of COVID-19?
Both tests are useful for managing the COVID-19 pandemic, so long as they’re used in the right way. The RNA test can rapidly identify which patients might be contagious, so they can be quarantined and the people with whom they’ve come in contact can be traced. Antibody tests can’t detect early stage disease, so they aren’t useful for effectively isolating new cases, but they can identify which people have encountered the virus previously and might be protected against it. Based on what we know about COVID-19 so far, many of these people will be immune, though it’s important to note that a positive antibody test doesn’t necessarily mean the person is not contagious. Even someone who is immune to having disease can be a short-term carrier as they fight off the virus. Anyone who tests positive for COVID-19, through either test, should follow CDC guidelines to prevent spreading the disease to others.
The RNA test can rapidly identify which patients might be contagious, so they can be quarantined and the people with whom they’ve come in contact can be traced. Antibody tests can’t detect early stage disease, so they aren’t useful for effectively isolating new cases, but they can identify which people have encountered the virus previously and might be protected against it. Based on what we know about COVID-19 so far, many of these people will be immune, though it’s important to note that a positive antibody test doesn’t necessarily mean the person is not contagious. Even someone who is immune to having disease can be a short-term carrier as they fight off the virus. Anyone who tests positive for COVID-19, through either test, should follow CDC guidelines to prevent spreading the disease to others.
I’ve seen COVID-19 tests referring to IgM, IgA and IgG. What do these terms mean?
Another name for antibody is immunoglobulin (Ig), and there are several different classes. Often, several types of antibodies are measured together to get a fuller picture of the immune landscape.
- • IgM antibodies are the first to appear to fight a new infection. They appear in the blood and often do not protect against infection.
• IgA antibodies are secreted into mucous and play a crucial role by preventing pathogens from taking up residence in the body.
• IgG antibodies are the most common type of antibody. They’re found in all bodily fluids and often provide long-term protection against the specific pathogen they’re built to fight. But we need to determine whether the IgG antibody that is detected by commercial COVID-19 tests is the type that protects against infection.