A “two-for-one” cancer immunotherapy is potentially more effective and at least as safe as standard immunotherapies, physician-scientists from UPMC Hillman Cancer Center who led an international, early-phase clinical trial report today in the journal Nature Medicine.
The findings, which involved hundreds of patients with different types of advanced solid tumors or blood cancers, point to an enticing new path for bispecific therapies that more efficiently unleash the patient’s own immune system to eliminate the cancer.
“No approved cancer drugs are like this. It is truly a novel development in the field,” said lead author Dr. Jason Luke, director of the Immunotherapy and Drug Development Center at UPMC Hillman and associate professor of hematology and oncology at the University of Pittsburgh School of Medicine. “The patients in our trial had cancers that were not responding to other therapies, so to see double-digit response rates is encouraging.”

Dr. Jason Luke
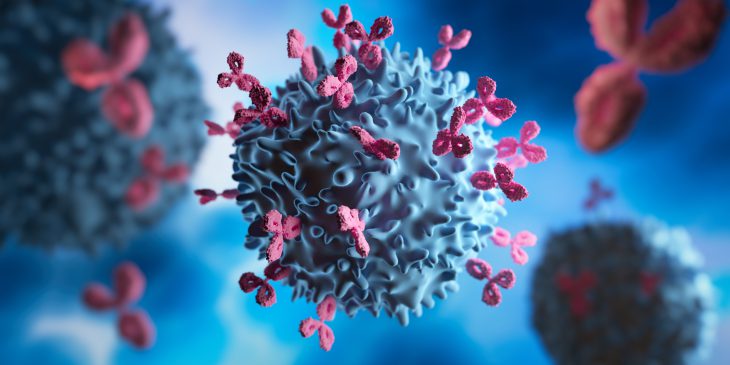
Some cancers proliferate when the patient’s immune system stops fighting them – in some cases because the cancer itself is turning off the immune response. The drug, tebotelimab, is a checkpoint inhibitor, meaning it prevents certain proteins released by tumors from binding to the surface of immune cells and telling them to stop responding to the cancer. Usually checkpoint inhibitor drugs target one immune system protein, but tebotelimab is bispecific and blocks two: PD-1 and LAG-3.
Drugs that block PD-1, such as pembrolizumab or nivolumab, have become a center point of treatment for many types of cancer. LAG-3 blocking drugs have recently been approved for advanced melanoma, but little clinical data exists to date for treatment of other types of cancer.
Luke says one drug doing the work of two may be better than two separate drugs, which might engage the immune system differently. When two drugs are used, they may not specifically bind together on the same immune cells. When one bispecific drug with two immune molecules binds to immune cells, the interactions are different and potentially generate greater immune activation.
In addition, the bispecific drug is not more toxic to the patient than one monospecific drug, whereas giving a patient two monospecific drugs typically would have added side effects.
The team enrolled 269 patients with advanced disease, including types of ovarian, breast, head and neck, cervical, and lymphoma cancers. Tumor size decreased in 34% of eligible participants.
The research team took the trial a step further and enrolled another 84 patients with advanced cancers positive for a protein called HER2 to test tebotelimab combined with an approved drug for HER2-positive cancer, called margetuximab. The response rate in those participants was 19%, which Luke said was impressive given the response rate is usually closer to 0% in these particular patients.
Luke says the next step is to develop a biomarker test that will tell doctors which patients have cancers that are expressing the proteins that tebotelimab is designed to block and then conduct another trial to see if outcomes are improved further. Additionally, future trials could test the immunotherapy in combination with chemotherapy or radiation.
“The early suggestion of response across multiple cancer types is intriguing,” said Luke. “This deserves further study, especially since this early phase trial gave us much more certainty around the safety of tebotelimab.”
This research was sponsored by MacroGenics, which is developing tebotelimab.
Journalists interested in learning more can contact mediarelations@upmc.edu.