A protein called PINK1 promotes complex branching of neurons in mice, according to a new study that could explain why Parkinson’s disease patients with mutations in the PINK1 gene often have cognitive impairment.
The findings by University of Pittsburgh researchers, published in The Journal of Neuroscience, may also help explain how neurodegeneration progresses in other diseases such as Alzheimer’s and could eventually point to new treatment approaches.

Dr. Charleen T. Chu
“We’re really excited about these findings because we show that PINK1 has an impact specifically on neuron structure and function, which we think could lead to a better understanding of why neurons degenerate and how we can prevent or reverse that process,” said senior author Dr. Charleen T. Chu, who holds the A. Julio Martinez chair in neuropathology and is a professor of pathology in the Pitt School of Medicine.
Parkinson’s disease is driven by loss of neurons in the substantia nigra, a brain region that regulates movement, leading to trembling or shaking, stiffness and problems with balance and coordination. The genetic and environmental causes of Parkinson’s are complex and not fully understood, but several different genes have been linked with development of the disease.
Beyond motor symptoms of Parkinson’s, some patients also experience cognitive issues related to memory and attention, develop psychiatric or mood disorders, and have increased risk of developing dementia. These symptoms occur in patients with two mutated copies of the PINK1 gene and also in family members with a mutation in only one copy of the gene, suggesting that this protein plays a key role in brain function.
To learn more about PINK1 in neurons, Chu and her team studied mice that lack expression of the PINK1 gene. Using a microscope, they looked at the tree-like branches called dendrites that extend out from the neuron to receive signals.
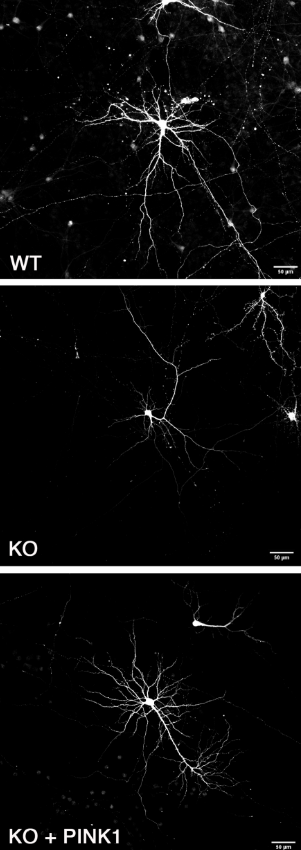
In normal mice (top image), neuron dendrites are intricately branched. In mice lacking the gene encoding a protein called PINK1 (middle image), there is a dramatic simplification of dendrite branching. When the researchers reintroduced PINK1 to neurons lacking the gene (bottom image), complex dendritic branching was restored (CREDIT: J. Neurosci 2022; 10.1523/JNEUROSCI.0785-22.2022)
Each neuron in the brain may be connected to thousands of other neurons. The more dense and intricate a neuron’s branches, the more connections called synapses it makes with other neurons, allowing better flow of information through the brain via electrical impulses. Simplification of this branching and loss of synaptic connections are associated with cognitive decline.
In normal mice, dendrites were intricately branched like a bushy, overgrown shrub. But in the mice that didn’t produce PINK1, the branches were less complex, as though the shrub had been pruned by an overzealous gardener.
The researchers also zoomed in to look at projections called dendritic spines, the structures that form a synapse with the end of other neurons. Like an unripe bud that unfurls into a leaf, dendritic spines begin as slender, hair-shaped structures called filopodia before swelling and finally maturing into toadstool-shaped mushroom spines.
“In neurons from the cortex of animals that lacked PINK1, we saw a decrease in the number of spines overall as well as altered distribution in the type of spines,” explained Chu, who is also a member of the McGowan Institute for Regenerative Medicine at Pitt. “We saw a shift from mushroom spines – which support strong neuronal connections and are important for memory — to filopodia, which are not yet functional.”
As a result of altered spine density and distribution, the electrical firing of these neurons was decreased, pointing to diminished connections between brain cells in the absence of PINK1.
When the researchers reintroduced human PINK1 to mouse neurons that lacked the protein, dendritic branching, spine density and neuron firing were restored to levels seen in normal neurons, confirming the importance of this protein for healthy neuron structure and function in both rodents and humans.
The next step for Chu and her team is to learn more about how PINK1 regulates dendritic branching and spine development. This research could eventually lead to new treatments to prevent or treat neurodegeneration in Parkinson’s and other diseases associated with reduced PINK1 expression such as some forms of Alzheimer’s.









