The body’s first line of defense against tuberculosis (TB) involves immune cells that suppress lung inflammation instead of activating it, reported University of Pittsburgh and the Ragon Institute of Mass General, MIT, and Harvard scientists today in Immunity. This is contrary to the immune system’s typical, pro-inflammatory response to infection.
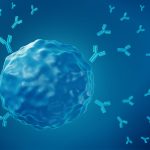
The research showed that a subset of infection-fighting white blood cells, called CD4 T cells, protect the lungs from reinfection by creating an anti-inflammatory environment within the lung tissue, rather than secreting molecules that directly kill invading Mycobacterium tuberculosis, or Mtb, bacteria that cause TB.
The unexpected discovery complements previous research about the role of protective immune T cells in controlling TB infection and points at ways to improve existing tuberculosis vaccines.

Dr. JoAnne Flynn
“Our study suggests that a vaccine that induces the ‘right’ kind of CD4 T cells that limit inflammation quickly upon infection may be key to providing long lasting immunity,” said senior and corresponding author Dr. JoAnne Flynn, distinguished professor and chair of microbiology and molecular genetics at Pitt.
Despite TB being all but eradicated in the United States, an estimated 10.6 million people globally fell ill with the disease in 2022. TB remains especially prevalent and deadly in Southeast Asia, Africa and the Western Pacific, where outbreaks occur regularly and people often get exposed to Mtb multiple times, even after the initial infection was cured.
Mtb infection is often accompanied by symptoms such as persistent cough, extreme exhaustion and fever, and it can cause lung inflammation and scarring. Yet, despite its significant public health burden, the disease has not been eradicated – largely due to relative ineffectiveness of the existing vaccine, Bacille Calmette-Guerin (BCG), which can protect young infants but not adults.
The development of better vaccines has been limited by an imperfect understanding of the dynamic interplay between Mtb and the host’s immune system and how Mtb evades immune response.
In the new study, researchers explored whether CD4 T cells are essential for protection. Surprisingly for Flynn, instead of observing that CD4 T lymphocytes secreted molecules that attract other infection-fighting cells to the sites of the Mtb invasion, CD4 cells instead contained the inflammation, making the infection site less hospitable to the bacteria.
The team showed that this process is mediated in part by the effects of CD4 T cells on CD8 T cells – another subset of white blood immune cells whose main function is killing cells infected by viruses. They concluded that the interplay between CD4 and CD8 T cells creates an anti-inflammatory environment that is hostile to Mtb and, as a result, limits bacterial growth and disease severity.
The expanded understanding of the role of CD4 T cells in preventing tuberculosis could provide new strategies for vaccine development.
“Our work demonstrates that control of TB requires a complex and sophisticated interplay of immune factors,” said Flynn. “Vaccine strategies have focused on inducing inflammatory CD4 T cells, but it might be time to shift our focus to reducing inflammation to the minimum level needed to limit growth of the bacteria, which will involve anti-inflammatory CD8 T cells and other cell types early on in infection”.