University of Pittsburgh School of Medicine researchers uncovered a fundamental mechanism that controls the body’s response to limited oxygen and regulates blood vessel disease of the lung.
By combing through genomes of more than 20,000 individuals in the U.S., France, England and Japan and combining the results with molecular studies in the lab, the team discovered a shared genetic trait that could predict a higher risk of small lung vessel disease called pulmonary hypertension and its more severe form, pulmonary arterial hypertension, and influence the development of drug therapies that target the body’s response to limited oxygen. The findings were published this week in Science Translational Medicine.
“This new level of knowledge will help identify people who may be at a higher genetic risk of pulmonary hypertension and jump-start precision medicine practices to offer customized treatments,” said senior author Dr. Stephen Chan, a cardiologist who serves as the Vitalant Chair in Vascular Medicine and director of the Vascular Medicine Institute at Pitt.

Stephen Chan, MD, PhD
Pulmonary hypertension encompasses a range of conditions of various causes that manifest in high blood pressure in the arteries of the lung and the right side of the heart. The disease is accompanied by a decreased supply of oxygen to the lung tissue and the blood, is chronic and deadly, and its molecular origins and genetic background remain unsolved.
Using a combined approach of genomics and biochemistry, the Chan lab found a gene pair that had an important function in regulating blood vessel metabolism and disease. This gene pair included a long non-coding RNA molecule – a messenger that facilitates the transformation of the body’s genetic code into protein products — and a protein binding partner, and their interaction was frequently active in cells exposed to low oxygen compared to normal cells.
Taking the findings a step further, the team discovered that a single DNA letter change directing expression of this RNA-protein pair under low oxygen conditions was associated with a higher genetic risk of pulmonary hypertension across diverse patient populations.
According to Chan, pulmonary hypertension is a borderline orphan disease, and the limited number of patients with pulmonary hypertension makes it challenging to find genetic variations that are rare but still impactful enough to eclipse individual differences.
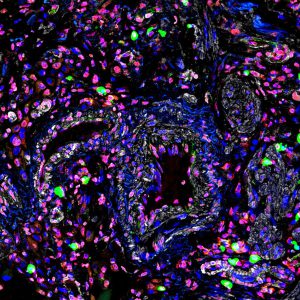
RNA fragments in a diseased lung vessel of a patient with pulmonary arterial hypertension.
With that in mind, Pitt scientists turned to collaborators around the globe and to public research datasets such as All of Us – a nationwide health registry funded by the National Institutes of Health – to ensure that the findings are relevant across a diverse global population.
Chan hopes that his findings will spur the development of targeted therapies relevant to oxygen sensitivity in blood vessel lining and that their pending patent application will contribute to the growth on an entirely new field of epigenetic and RNA drug therapeutics that work not by manipulating the genome but by changing how it is being read.
Journalists interested in learning more can contact mediarelations@upmc.edu.