This month’s issue of Psychology of Addictive Behaviorstakes on the important topic of how brain imaging research can help to improve psychotherapy for addictive behaviors.
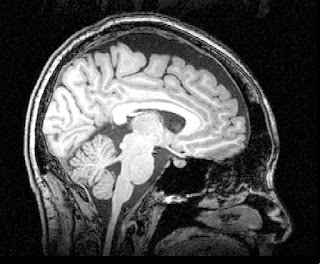
For some background, neuroimaging (brain imaging) includes a variety of methods that are used to examine brain structure and functioning. Brain imaging methods include:
- Magnetic Resonance Imaging (MRI): a widely used, non-invasive method that is generally safe (it does not involve radiation), and produces an image that looks like an x-ray.
- Structural MRI (sMRI): this can show various brain structures, including damage to brain tissue, such as lesions and tumors.
- Functional MRI (fMRI): this is used to study activity in specific brain regions, usually in response to a specific experimental task (e.g., seeing a flash of light).
- Diffusion Tensor Imaging (DTI): this is another popular, non-invasive and safe imaging method which can show white matter tracts in the brain that facilitate communication between brain regions.
The topic of the special issue of the journal was motivated by the urgent need to improve treatment for addictive behaviors. Current psychotherapies for addictive behaviors are only moderately successful in helping people to “stay clean,” with relapse as a relatively common outcome. This modest success rate for treatment is partly due to our limited understanding of how and why psychotherapy works, particularly at the level of brain structure and functioning. The idea behind the special issue is that by understanding how effective psychotherapies have an impact on brain structure and functioning, we will be able to design more effective interventions with stronger and longer lasting effects.
Here, we ask Tammy Chung, Ph.D., Associate Professor of Psychiatry and Epidemiology at the University of Pittsburgh School of Medicine, to answer a few questions about the journal’s special issue, titled “Neuroimaging psychotherapy mechanisms of change for addictive behaviors”.
Q: What exactly does “psychotherapy mechanisms of change for addictive behaviors” mean, and how does neuroimaging play a role?
A: A “mechanism of change” explains how a treatment works. For example, in cognitive behavioral therapy (CBT), a proposed “active ingredient” that explains how the therapy works is the development of skills to cope with craving, such as actively seeking social support for abstinence, rather than giving in to the urge to use. Effective use of coping skills might involve an increase in the activation of brain areas that are associated with the regulation of behavior, such as the prefrontal cortex (an area of the brain just behind the forehead). Neuroimaging could play an important role in helping us to understand how this “active ingredient” of treatment works by showing, for example, that effective treatment increased activation (compared to before treatment) in an area of the brain associated with the regulation of behavior and emotions, which in turn was associated with better outcomes. Understanding the brain-based mechanisms underlying successful recovery is critical to designing and delivering effective treatment.
Q: How can neuroimaging help us to understand the science of addiction?
A: So far, neuroimaging studies have shown that chronic, heavy substance users, compared to their healthy counterparts (same age and sex), show deficits in brain structure. For example, alcoholic patients have smaller regional brain volumes, likely due to heavy alcohol use, compared to healthy adults. Chronic substance users also tend to show alterations in brain functioning. As an example, chronic substance users typically show less activation in brain regions (e.g., in the prefrontal cortex) that are associated with the ability to effectively control behavior and regulate emotions. It’s not clear how much these differences are due to heavy substance use, or if they existed prior to heavy substance use. However, emerging research suggests that youth at high risk for substance use show less activation in brain regions associated with behavioral control, even before starting substance use. But we still don’t know a lot about how the brain changes in response to psychotherapy.
Q: How can neuroimaging help us predict which treatments will work and which will be less effective?
A: We’re only starting to understand the potential of neuroimaging to help us predict which treatments will work, and for whom they will work best. One of the studies in the special issue found that greater integrity of white matter in the prefrontal cortex, a region associated with the ability to regulate behavior, predicted lower severity of alcohol problems following treatment in adolescents. This result suggests that there are brain-based characteristics at the start of treatment that could predict better outcome. The result also suggests that finding ways to improve white matter integrity, such as exercise and nutrition, and maintaining abstinence from substance use, are important treatment goals.
Q: What was the goal of this special journal issue?
A: Treatment researchers are not usually trained in neuroimaging (but that may change!), and few neuroimaging researchers specialize in addictions treatment (which we hope will change!). The special issue was intended to foster collaboration between two fairly specialized areas, to begin to understand the process by which psychotherapy, which can be thought of as a specialized form of learning, has an impact at the level of brain structure and functioning. Understanding changes at the level of the brain could inspire novel treatment methods that target specific brain-based mechanisms that underlie sustained recovery from addiction.